Research Report Series: Nicotine Addiction
Download PDF Version What is PDF?
Source: NIDA Research Report Series: Nicotine Addiction, NIH Publication Number 01-4342, July, 1998
Public Domain
Table of Contents (TOC)
From the DirectorChapter 1: What is nicotine?
Chapter 2: Is nicotine addictive?
Chapter 3: What is the extent and impact of tobacco use?
Chapter 4: How does nicotine deliver its effect?
Chapter 5: What happens when nicotine is taken for long periods of time?
Chapter 6: What are the medical consequences of nicotine use?
Chapter 7: Smoking and pregnancy: What are the risks?
Chapter 8: Are there effective treatments for nicotine addiction?
Chapter 9: Are there gender differences in tobacco smoking?
Glossary
References
The use of tobacco products may be the Nation’s most critical public health problem. It is, in fact, addiction to nicotine that is at the root of this enormous health, social, and financial burden.
 An improved overall understanding of addiction, coupled with the identification
of nicotine as an addictive drug, has been instrumental in the development
of medications and behavioral treatments for nicotine addiction. In
essence, science-driven treatment development has provided to consumers
the option to easily purchase effective treatments, such as the nicotine
patch and nicotine gum, in their local drugstores and supermarkets.
Science has also shown that treating addiction with medications alone
is not nearly as effective as when the medication is coupled with a
behavioral approach. While we have made substantial progress in developing
both pharmacological and behavioral treatments that have proven effective
for many people, much more remains to be done.
An improved overall understanding of addiction, coupled with the identification
of nicotine as an addictive drug, has been instrumental in the development
of medications and behavioral treatments for nicotine addiction. In
essence, science-driven treatment development has provided to consumers
the option to easily purchase effective treatments, such as the nicotine
patch and nicotine gum, in their local drugstores and supermarkets.
Science has also shown that treating addiction with medications alone
is not nearly as effective as when the medication is coupled with a
behavioral approach. While we have made substantial progress in developing
both pharmacological and behavioral treatments that have proven effective
for many people, much more remains to be done.
Through the use of advanced neuroimaging technologies, we are now actually able to see some of the changes in brain function that occur as people smoke tobacco products. Researchers are beginning to find that there may be chemicals other than nicotine in cigarette smoke that contribute to tobacco’s addictiveness. This finding and many other new research accomplishments in the addiction arena are providing us with an unprecedented opportunity to curtail this enormous public health crisis. We hope this compilation of scientific information will help to inform readers about our current understanding of nicotine addiction and its harmful effects and will assist in prevention and treatment efforts.
Alan I. Leshner, Ph.D.
Director
National Institute on Drug Abuse
 Nicotine, one of more than 4,000 chemicals found in the
smoke from tobacco products such as cigarettes, cigars,
and pipes, is the primary component in tobacco that acts
on the brain. Smokeless tobacco products such as snuff and
chewing tobacco also contain many toxins as well as high
levels of nicotine. Nicotine, recognized as one of the most
frequently used addictive drugs, is a naturally occurring
colorless liquid that turns brown when burned and acquires
the odor of tobacco when exposed to air. There are many
species of tobacco plants; the tabacum species serves as
the major source of tobacco products today. Since nicotine
was first identified in the early 1800s, it has been studied
extensively and shown to have a number of complex and sometimes
unpredictable effects on the brain and the body.
Nicotine, one of more than 4,000 chemicals found in the
smoke from tobacco products such as cigarettes, cigars,
and pipes, is the primary component in tobacco that acts
on the brain. Smokeless tobacco products such as snuff and
chewing tobacco also contain many toxins as well as high
levels of nicotine. Nicotine, recognized as one of the most
frequently used addictive drugs, is a naturally occurring
colorless liquid that turns brown when burned and acquires
the odor of tobacco when exposed to air. There are many
species of tobacco plants; the tabacum species serves as
the major source of tobacco products today. Since nicotine
was first identified in the early 1800s, it has been studied
extensively and shown to have a number of complex and sometimes
unpredictable effects on the brain and the body.
Cigarette smoking is the most prevalent form of nicotine addiction in the United States. Most cigarettes in the U.S. market today contain 10 milligrams (mg) or more of nicotine. Through inhaling smoke, the average smoker takes in 1 to 2 mg nicotine per cigarette. There have been substantial increases in the sale and consumption of smokeless tobacco products also, and more recently, in cigar sales.
Nicotine is absorbed through the skin and mucosal lining of the mouth and nose or by inhalation in the lungs. Depending on how tobacco is taken, nicotine can reach peak levels in the bloodstream and brain rapidly. Cigarette smoking, for example, results in rapid distribution of nicotine throughout the body, reaching the brain within 10 seconds of inhalation. Cigar and pipe smokers, on the other hand, typically do not inhale the smoke, so nicotine is absorbed more slowly through the mucosal membranes of their mouths. Nicotine from smokeless tobacco also is absorbed through the mucosal membranes.
Yes, nicotine is addictive. Most smokers use tobacco regularly because they are addicted to nicotine. Addiction is characterized by compulsive drug-seeking and use, even in the face of negative health consequences, and tobacco use certainly fits the description. It is well documented that most smokers identify tobacco as harmful and express a desire to reduce or stop using it, and nearly 35 million of them make a serious attempt to quit each year. Unfortunately, less than 7 percent of those who try to quit on their own achieve more than 1 year of abstinence; most relapse within a few days of attempting to quit.
Other factors to consider besides nicotine’s addictive properties include its high level of availability, the small number of legal and social consequences of tobacco use, and the sophisticated marketing and advertising methods used by tobacco companies. These factors, combined with nicotine’s addictive properties, often serve as determinants for first use and, ultimately, addiction.
Trends in percent of adolescents reporting current* cigarette use
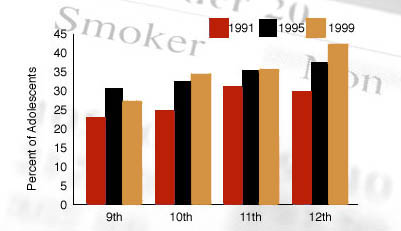
*Individual with reports smoking one or more cigarettes during the previous 30 days.
Source: CDC, MMWR, 2000; 49(33): 755-758
Recent research has shown in fine detail how nicotine acts on the brain to produce a number of behavioral effects. Of primary importance to its addictive nature are findings that nicotine activates the brain circuitry that regulates feelings of pleasure, the so-called reward pathways. A key brain chemical involved in mediating the desire to consume drugs is the neurotransmitter dopamine, and research has shown that nicotine increases the levels of dopamine in the reward circuits. Nicotine’s pharmacokinetic properties have been found also to enhance its abuse potential. Cigarette smoking produces a rapid distribution of nicotine to the brain, with drug levels peaking within 10 seconds of inhalation. The acute effects of nicotine dissipate in a few minutes, causing the smoker to continue dosing frequently throughout the day to maintain the drug’s pleasurable effects and prevent withdrawal.
 What people frequently do not realize is that the cigarette is a very
efficient and highly engineered drug-delivery system. By inhaling,
the smoker can get nicotine to the brain very rapidly with every puff.
A typical smoker will take 10 puffs on a cigarette over a period of
5 minutes that the cigarette is lit. Thus, a person who smokes about
1-1/2 packs (30 cigarettes) daily, gets 300 "hits" of nicotine to the
brain each day. These factors contribute considerably to nicotine’s
highly addictive nature.
What people frequently do not realize is that the cigarette is a very
efficient and highly engineered drug-delivery system. By inhaling,
the smoker can get nicotine to the brain very rapidly with every puff.
A typical smoker will take 10 puffs on a cigarette over a period of
5 minutes that the cigarette is lit. Thus, a person who smokes about
1-1/2 packs (30 cigarettes) daily, gets 300 "hits" of nicotine to the
brain each day. These factors contribute considerably to nicotine’s
highly addictive nature.
Scientific research is also beginning to show that nicotine may not be the only psychoactive ingredient in tobacco. Using advanced neuroimaging technology, scientists can see the dramatic effect of cigarette smoking on the brain and are finding a marked decrease in the levels of monoamineoxidase (MAO), an important enzyme that is responsible for breaking down dopamine. The change in MAO must be caused by some tobacco smoke ingredient other than nicotine, since we know that nicotine itself does not dramatically alter MAO levels. The decrease in two forms of MAO, A and B, then results in higher dopamine levels and may be another reason that smokers continue to smoke - to sustain the high dopamine levels that result in the desire for repeated drug use.
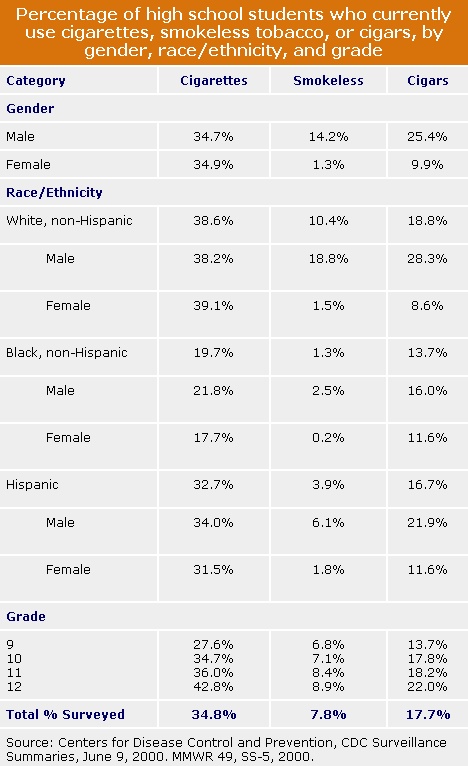
According to the 1999 National Household Survey on Drug Abuse, an estimated 57.0 million Americans were current smokers and 7.6 million used smokeless tobacco, which means that nicotine is one of the most widely abused substances. In addition, in 1998 each day in the United States more than 2,000 people under the age of 18 began daily smoking. According to the Centers for Disease Control and Prevention (CDC), the prevalence of cigarette smoking among U.S. high school students increased from 27.5 percent in 1991 to 36.4 percent in 1997 before declining to 34.8 percent in 1999. NIDA’s own Monitoring the Future Study, which annually surveys drug use and related attitudes of America’s adolescents, also found the prevalence rates for smoking among youth declined from 1999 to 2000. Since 1975, nicotine in the form of cigarettes has consistently been the substance the greatest number of high school students use daily.
The impact of nicotine addiction in terms of morbidity, mortality, and economic costs to society is staggering. Tobacco kills more than 430,000 U.S. citizens each year-more than alcohol, cocaine, heroin, homicide, suicide, car accidents, fire, and AIDS combined. Tobacco use is the leading preventable cause of death in the United States.
Economically, an estimated $80 billion of total U.S. health care costs each year is attributable to smoking. However, this cost is well below the total cost to society because it does not include burn care from smoking-related fires, perinatal care for low-birth-weight infants of mothers who smoke, and medical care costs associated with disease caused by secondhand smoke. Taken together, the direct and indirect costs of smoking are estimated at $138 billion per year.
 Nicotine can act as both a stimulant and a sedative. Immediately
after exposure to nicotine, there is a "kick" caused in
part by the drug’s stimulation of the adrenal glands and
resulting discharge of epinephrine (adrenaline). The rush
of adrenaline stimulates the body and causes a sudden release
of glucose as well as an increase in blood pressure, respiration,
and heart rate. Nicotine also suppresses insulin output
from the pancreas, which means that smokers are always slightly
hyperglycemic. In addition, nicotine indirectly causes a
release of dopamine in the brain regions that control pleasure
and motivation. This reaction is similar to that seen with
other drugs of abuse-such as cocaine and heroin- and it
is thought to underlie the pleasurable sensations experienced
by many smokers. In contrast, nicotine can also exert a
sedative effect, depending on the level of the smoker’s
nervous system arousal and the dose of nicotine taken.
Nicotine can act as both a stimulant and a sedative. Immediately
after exposure to nicotine, there is a "kick" caused in
part by the drug’s stimulation of the adrenal glands and
resulting discharge of epinephrine (adrenaline). The rush
of adrenaline stimulates the body and causes a sudden release
of glucose as well as an increase in blood pressure, respiration,
and heart rate. Nicotine also suppresses insulin output
from the pancreas, which means that smokers are always slightly
hyperglycemic. In addition, nicotine indirectly causes a
release of dopamine in the brain regions that control pleasure
and motivation. This reaction is similar to that seen with
other drugs of abuse-such as cocaine and heroin- and it
is thought to underlie the pleasurable sensations experienced
by many smokers. In contrast, nicotine can also exert a
sedative effect, depending on the level of the smoker’s
nervous system arousal and the dose of nicotine taken.
Chronic exposure to nicotine results in addiction. Research is just beginning to document all of the neurological changes that accompany the development and maintenance of nicotine addiction. The behavioral consequences of these changes are well documented, however. Greater than 90 percent of those smokers who try to quit without seeking treatment fail, with most relapsing within a week.
Repeated exposure to nicotine results in the development of tolerance, the condition in which higher doses of a drug are required to produce the same initial stimulation. Nicotine is metabolized fairly rapidly, disappearing from the body in a few hours. Therefore some tolerance is lost overnight, and smokers often report that the first cigarettes of the day are the strongest and/or the "best." As the day progresses, acute tolerance develops, and later cigarettes have less effect.
 Cessation of nicotine use is followed by a withdrawal syndrome
that may last a month or more; it includes symptoms that
can quickly drive people back to tobacco use. Nicotine withdrawal
symptoms include irritability, craving, cognitive and attentional
deficits, sleep disturbances, and increased appetite and
may begin within a few hours after the last cigarette. Symptoms
peak within the first few days and may subside within a
few weeks. For some people, however, symptoms may persist
for months or longer.
Cessation of nicotine use is followed by a withdrawal syndrome
that may last a month or more; it includes symptoms that
can quickly drive people back to tobacco use. Nicotine withdrawal
symptoms include irritability, craving, cognitive and attentional
deficits, sleep disturbances, and increased appetite and
may begin within a few hours after the last cigarette. Symptoms
peak within the first few days and may subside within a
few weeks. For some people, however, symptoms may persist
for months or longer.
An important but poorly understood component of the nicotine withdrawal syndrome is craving, an urge for nicotine that has been described as a major obstacle to successful abstinence. High levels of craving for tobacco may persist for 6 months or longer. While the withdrawal syndrome is related to the pharmacological effects of nicotine, many behavioral factors also can affect the severity of withdrawal symptoms. For some people, the feel, smell, and sight of a cigarette and the ritual of obtaining, handling, lighting, and smoking the cigarette are all associated with the pleasurable effects of smoking and can make withdrawal or craving worse. While nicotine gum and patches may alleviate the pharmacological aspects of withdrawal, cravings often persist.
The medical consequences of nicotine exposure result from effects of both the nicotine itself and how it is taken. The most deleterious effects of nicotine addiction are the result of tobacco use, which accounts for one-third of all cancers. Foremost among the cancers caused by tobacco is lung cancer-the number one cancer killer of both men and women. Cigarette smoking has been linked to about 90 percent of all lung cancer cases.
In addition to lung cancer, smoking also causes lung diseases such as chronic bronchitis and emphysema, and it has been found to exacerbate asthma symptoms in adults and children. Smoking is also associated with cancers of the mouth, pharynx, larynx, esophagus, stomach, pancreas, cervix, kidney, ureter, and bladder. The overall rates of death from cancer are twice as high among smokers as among nonsmokers, with heavy smokers having rates that are four times greater than those of nonsmokers. Cigarette smoking is the most important preventable cause of cancer in the United States.
430,000 annual deaths are attributable to cigarette smoking
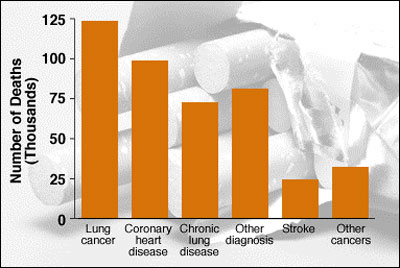
Source: CDC, MMWR 1997; 46; 448-51
In addition to its ability to cause cancer, a relationship between cigarette smoking and coronary heart disease was first reported in the 1940s. Since that time, it has been well documented that smoking substantially increases the risk of heart disease, including stroke, heart attack, vascular disease, and aneurysm. It is estimated that nearly one-fifth of deaths from heart disease are attributable to smoking.
While we often think of medical consequences that result from direct use of tobacco products, passive or secondary smoke also increases the risk for many diseases. Environmental tobacco smoke (ETS) is a major source of indoor air contaminants; secondhand smoke is estimated to cause approximately 3,000 lung cancer deaths per year among nonsmokers and contributes to as many as 40,000 deaths related to cardiovascular disease. Exposure to tobacco smoke in the home increases the severity of asthma for children and is a risk factor for new cases of childhood asthma. ETS exposure has been linked also with sudden infant death syndrome. Additionally, dropped cigarettes are the leading cause of residential fire fatalities, leading to more than 1,000 such deaths each year.
 At higher doses, such as the nicotine that can be found in some insecticide
sprays, nicotine can be extremely toxic, causing vomiting,
tremors, convulsions, and death. Nicotine poisoning has been reported
from accidental ingestion of insecticides by adults and ingestion of
tobacco products by children and pets. Death usually results in a few
minutes from respiratory failure caused by paralysis.
At higher doses, such as the nicotine that can be found in some insecticide
sprays, nicotine can be extremely toxic, causing vomiting,
tremors, convulsions, and death. Nicotine poisoning has been reported
from accidental ingestion of insecticides by adults and ingestion of
tobacco products by children and pets. Death usually results in a few
minutes from respiratory failure caused by paralysis.
Laboratory research indicates that cigarette smoking causes toxic cardiovascular effects. For this reason, nicotine replacement medicines such as nicotine gum and the patch have been extensively evaluated for cardiovascular toxicity, especially for patients with cardiac disease. These trials suggest that use of nicotine replacements for smoking cessation does not increase cardiovascular risk. These findings are consistent with the generally slower and lower doses of nicotine obtained from the medicines as compared to tobacco products, and to the absence of carbon monoxide and numerous other toxins in tobacco smoke.
In pregnant women, carbon monoxide (a lethal gas) and the high doses of nicotine obtained when they inhale tobacco smoke interferes with oxygen supply to the fetus. Nicotine readily crosses the placenta, and nicotine concentrations in the fetus can be as much as 15 percent higher than maternal levels. It appears that nicotine is concentrated in fetal blood, amniotic fluid, and breast milk. Another ingredient of tobacco smoke, carbon monoxide, has been shown to inhibit the release of oxygen into fetal tissues. These factors, combined, likely account for the developmental delays commonly seen in the fetuses and infants of smoking mothers.
 Women who smoke during pregnancy are at greater risk than nonsmokers
for premature delivery, and there is a risk of lower birth weight for
infants carried to term. In the United States it is estimated that 20
percent or more of pregnant women smoke throughout their pregnancies.
The adverse effects of smoking may occur in every trimester of pregnancy;
they range from spontaneous abortions in the first trimester to increased
premature delivery rates and decreased birth weights in the final trimester.
The decreased birth weights seen in infants of mothers who smoke reflects
a dose-dependent relationship: the more the woman smokes during pregnancy,
the greater the reduction of infant birth weight. Conversely, women who
give up smoking early in pregnancy have infants of similar weight to
those of nonsmokers.
Women who smoke during pregnancy are at greater risk than nonsmokers
for premature delivery, and there is a risk of lower birth weight for
infants carried to term. In the United States it is estimated that 20
percent or more of pregnant women smoke throughout their pregnancies.
The adverse effects of smoking may occur in every trimester of pregnancy;
they range from spontaneous abortions in the first trimester to increased
premature delivery rates and decreased birth weights in the final trimester.
The decreased birth weights seen in infants of mothers who smoke reflects
a dose-dependent relationship: the more the woman smokes during pregnancy,
the greater the reduction of infant birth weight. Conversely, women who
give up smoking early in pregnancy have infants of similar weight to
those of nonsmokers.
Yes, extensive research has shown that behavioral and pharmacological treatments for nicotine addiction do work. For those individuals motivated to quit smoking, a combination of behavioral and pharmacological treatments can increase the success rate approximately twofold over placebo treatments. Furthermore, smoking cessation can have an immediate positive impact on an individual’s health; for example, a 35-year-old man who quits smoking will, on the average, increase his life expectancy by 5.1 years.
Nicotine Replacement Treatments
Nicotine was the first pharmacological agent approved by the Food and Drug Administration (FDA) for use in smoking cessation therapy. Nicotine replacement therapies, such as nicotine gum, the transdermal patch, nasal spray, and inhaler, have been approved for use in the United States. They are used to relieve withdrawal symptoms, because they produce less severe physiological alterations than tobacco-based systems, and generally provide users with lower overall nicotine levels than they receive with tobacco. An added benefit is that these forms of nicotine have little abuse potential since they do not produce the pleasurable effects of tobacco products. Nor do they contain the carcinogens and gases associated with tobacco smoke.
The FDA’s approval of nicotine gum in 1984 marked the availability (by prescription) of the first nicotine replacement therapy on the U.S. market. In 1996, the FDA approved gum (Nicorette®) for over-the-counter sales. Whereas nicotine gum provides some smokers with the desired control over dose and ability to relieve cravings, others are unable to tolerate the taste and chewing demands. In 1991-1992, FDA approved four transdermal nicotine patches, two of which became over-the-counter products in 1996, thus meeting the needs of many additional tobacco users.
 Since the introduction of nicotine gum and the transdermal
patch, estimates based on FDA and pharmaceutical
industry data indicate that more than 1 million individuals
have been successfully treated for nicotine addiction.
In 1996 a nicotine nasal spray, and in 1998 a nicotine
inhaler, became available by prescription. All the
nicotine replacement products- gum, patch, spray
and inhaler- appear to be equally effective. In fact,
the over-the-counter availability of many of these
medications, combined with increased messages to
quit smoking in the media, has produced about a 20
percent increase in successful quitting each year.
Since the introduction of nicotine gum and the transdermal
patch, estimates based on FDA and pharmaceutical
industry data indicate that more than 1 million individuals
have been successfully treated for nicotine addiction.
In 1996 a nicotine nasal spray, and in 1998 a nicotine
inhaler, became available by prescription. All the
nicotine replacement products- gum, patch, spray
and inhaler- appear to be equally effective. In fact,
the over-the-counter availability of many of these
medications, combined with increased messages to
quit smoking in the media, has produced about a 20
percent increase in successful quitting each year.
Non-Nicotine Therapies
Although the major focus of pharmacological treatments of nicotine addiction has been nicotine replacement, other treatments are being developed for relief of nicotine withdrawal symptoms. For example, the first non-nicotine prescription drug, bupropion, an antidepressant marketed as Zyban®, has been approved for use as a pharmacological treatment for nicotine addiction. In December 1996, a Federal advisory committee recommended that the FDA approve bupropion to become the first drug to help people quit smoking that could be taken in pill form, and the first to contain no nicotine.
Behavioral Treatments
Behavioral interventions can play an integral role in nicotine addiction treatment. Over the past decade, this approach has spread from primarily clinic-based, formal smoking-cessation programs to application in numerous community and public health settings, and now to telephone and written formats as well. In general, behavioral methods are employed to (a) discover high-risk relapse situations, (b) create an aversion to smoking, (c) develop self-monitoring of smoking behavior, and (d) establish competing coping responses.
 Other key factors in successful treatment include
avoiding smokers and smoking environments and receiving
support from family and friends. The single most
important factor, however, may be the learning and
use of coping skills for both short- and long-term
prevention of relapse. Smokers must not only learn
behavioral and cognitive tools for relapse prevention
but must also be ready to apply those skills in a
crisis.
Other key factors in successful treatment include
avoiding smokers and smoking environments and receiving
support from family and friends. The single most
important factor, however, may be the learning and
use of coping skills for both short- and long-term
prevention of relapse. Smokers must not only learn
behavioral and cognitive tools for relapse prevention
but must also be ready to apply those skills in a
crisis.
Although behavioral and pharmacological treatments can be extremely successful when employed alone, science has taught us that integrating both types of treatments will ultimately be the most effective approach. More than 90 percent of the people who try to quit smoking relapse or return to smoking within 1 year, with the majority relapsing within a week. There are, however, an estimated 2.5 to 5 percent who do in fact succeed on their own. It has been shown that pharmacological treatments can double the odds of their success. However, a combination of pharmacological and behavioral treatments further improves their chances. For example, when use of the nicotine patch is combined with a behavioral approach, such as group therapy or social support networks, the efficacy of treatment is significantly enhanced.
Several avenues of research now indicate that men and women differ in their smoking behavior and that differences in nicotine sensitivity may be the root cause. Studies of smoking behavior seem to indicate that women smoke fewer cigarettes per day, tend to use cigarettes with lower nicotine content, and do not inhale as deeply as men. Whether this is because of differences in sensitivity to nicotine is an important research question. Some researchers are finding that women may be more affected by factors other than nicotine, such as the sensory aspects of the smoke or social factors, than they are by nicotine itself.
The number of smokers in the United States declined in the 1970s and 1980s, but has been relatively stable throughout the 1990s. Because this decline of smoking was greater among men than women, the prevalence of smoking is only slightly higher for men today than it is for women. Several factors appear to be contributing to this trend, including increased initiation of smoking among female teens and, more critically, women being less likely than men to quit smoking.
 Large-scale smoking-cessation trials show that women
are less likely to initiate quitting and may be more
likely to relapse if they do quit. In cessation programs
using nicotine replacement methods, such as the patch
or gum, the nicotine does not seem to reduce craving
as effectively for women as for men. Other factors
that may contribute to women’s difficulty with quitting
are that the withdrawal syndrome may be more intense
for women and that they appear more likely than men
to gain weight upon quitting. It is important for
women entering smoking cessation programs to be aware
that standard treatment regimens may have to be adjusted
to compensate for gender differences in nicotine
sensitivity.
Large-scale smoking-cessation trials show that women
are less likely to initiate quitting and may be more
likely to relapse if they do quit. In cessation programs
using nicotine replacement methods, such as the patch
or gum, the nicotine does not seem to reduce craving
as effectively for women as for men. Other factors
that may contribute to women’s difficulty with quitting
are that the withdrawal syndrome may be more intense
for women and that they appear more likely than men
to gain weight upon quitting. It is important for
women entering smoking cessation programs to be aware
that standard treatment regimens may have to be adjusted
to compensate for gender differences in nicotine
sensitivity.
Addiction: A chronic, relapsing disease, characterized by compulsive drug-seeking and use and by neurochemical and molecular changes in the brain.
Adrenal glands: Glands located above each kidney that secrete hormones, e.g., adrenaline.
Craving: A powerful, often uncontrollable desire for drugs.
Dopamine: A neurotransmitter present in regions of the brain that regulate movement, emotion, motivation, and the feeling of pleasure.
Emphysema: A lung disease in which tissue deterioration results in increased air retention and reduced exchange of gases. The result is difficult breathing and shortness of breath. It is often caused by smoking.
Nicotine: An alkaloid derived from the tobacco plant that is responsible for smoking’s psychoactive and addictive effects; is toxic at high doses but can be safe and effective as medicine at lower doses.
Pharmacokinetics: The pattern of absorption, distribution, and excretion of a drug over time.
Physical dependence: An adaptive physiological state that occurs with regular drug use and results in a withdrawal syndrome when drug use is stopped; usually occurs with tolerance.
Rush: A surge of pleasure that rapidly follows administration of some drugs.
Tobacco: A plant widely cultivated for its leaves, which are used primarily for smoking; the tabacum species is the major source of tobacco products.
Tolerance: A condition in which higher doses of a drug are required to produce the same effect as during initial use; often leads to physical dependence.
Withdrawal: A variety of symptoms that occur after use of an addictive drug is reduced or stopped.
Bartecchi, C.E.; MacKenzie, T.D.; and Schrier, R.W. Human costs of tobacco use. New Engl J Med 330:907-980, 1994.
Benowitz, N.L. Pharmacology of nicotine: addiction and therapeutics. Ann Rev Pharmacol Toxicol 36:597-613, 1996.
Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report 49(33):755-758, 2000.
Centers for Disease Control and Prevention. CDC Surveillance Summaries, June 9, 2000. MMWR 49, SS-5, 2000.
Giovino, G.A.; Henningfield, J.E.; Tomar, S.L.; Escobedo, L.G.; and Slade, J. Epidemiology of tobacco use and dependence. Epidemiol Rev 17(1):48-65, 1995.
Henningfield, J.E. Nicotine medications for smoking cessation. New Engl J Med 333:1196-1203, 1995.
Hughes, J.R. The future of smoking cessation therapy in the United States. Addiction 91:1797-1802, 1996.
Lynch, B.S., and Bonnie, R.J., eds. Growing Up Tobacco Free. Preventing Nicotine Addiction in Children and Youths. Committee on Preventing Nicotine Addiction in Children and Youths. Division of Biobehavioral Sciences and Mental Disorders, Institute of Medicine, 1995.
Martin, W.R.; Van Loon, G.R.; Iwamoto, E.T.; and Davis, L., eds. Tobacco Smoking and Nicotine. New York: Plenum Publishing, 1987.
National Institute on Drug Abuse. Monitoring the Future, National Results on Adolescent Drug Use, Overview of Key Findings 2000. NIH Pub. No. 01-4923, 2001.
Pomerleau, O.F.; Collins, A.C.; Shiffman, S.; and Pomerleau, C.S. Why some people smoke and others do not: new perspectives. J Consult Clin Psychol 61:723-731, 1993.
Rice, D.P. Economic Costs of Substance Abuse, 1995. Proceedings of the Association of American Physicians, 111(2):119-125, 1999.
The Smoking Cessation Clinical Practice Guideline Panel and Staff. The Agency for Health Care Policy and Research smoking cessation clinical practice guidelines. JAMA 275:1270-1280, 1996.
Substance Abuse and Mental Health Services Administration. Summary of Findings from the 1999 National Household Survey on Drug Abuse. SAMHSA, 2000.


